The African American Breast Cancer Alliance (AABCA) raises critical breast cancer awareness and empowers Black women with lifesaving information.
In October 1990, nine Black women came together to discuss their personal experiences with breast cancer, creating the African American Breast Cancer Alliance (AABCA) in Minnesota. “The big C” was a silent foe in the community. There was no culturally specific information about breast cancer and Black women or that Black women are diagnosed younger than age 45 with aggressive breast cancers due to delays in detection for various reasons. Too many Black women of all ages are suffering and losing their lives from breast cancer due to health inequalities.
Currently, 1 in 12 Black women are diagnosed with breast cancer by age 80 during their lifetime, compared to the overall numbers of one in eight American women. Black women still hold the record for higher breast cancer death rates, although survival rates are increasing.
Raising awareness
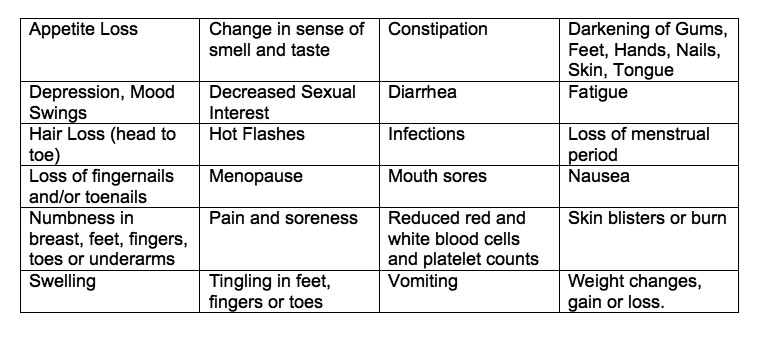
Black women are now more aware of breast cancer and why it is important for them to take action in their self and clinical breast examinations, and learn about their family cancer history and mammograms. However, action is not historically the first line for most Black women if they find unusual changes in their breast(s). Cancer treatments, disbelief, fear of death, lack of insurance, knowledge, myths, other health and lifestyle issues, plus socioeconomic issues still keep Black women from seeking the medical help they need. The emotional and physical toll of breast cancer treatments can stop a woman in her tracks, anticipating chemotherapy, surgeries, losing a breast, radiation therapy, etc. — effects that can actually be lifesaving. Sadly, fear of losing her hair, femininity, or life results in too many women dying needlessly.
For 32 years, the goal of the AABCA has been to educate and support Black women diagnosed with breast cancer, along with men, families, and communities. Because of the severe impact breast cancer has on the Black population, AABCA provides an emotional and social network through events and Zoom support groups. AABCA empowers people to reach out to “share, support, and survive” through the trials and tribulations of breast cancer.
It takes a community
Recently, funding from the Minnesota Timberwolves Fastbreak Foundation has helped increase AABCA’s efforts in awareness, and health and racial disparities that affect Black women. In addition, AABCA has collaborated with the Breast Believe campaign, led by The Larry Fitzgerald Foundation (TLFF), that aims to educate communities about early detection, prevention, symptoms, treatments, resources, and access surrounding a breast cancer diagnosis.
While October is Breast Cancer Awareness Month, not everything looks pretty in pink as more women and men are diagnosed with breast cancer, devastating families and our communities. As a two-time, 32-year breast cancer survivor, the ruthless road of this disease is never ending, claiming victims and taking no prisoners. But patients and survivors are taking on the fight one day at a time and living our lives the best we can.
If you or someone you know is dealing with breast cancer, feel free to contact us.